Introduction
Dental occlusion and the temporomandibular joint (TMJ) are fundamental pillars in dentistry. Their intricate biomechanical relationship governs oral function, structural stability, and overall patient well-being. A deep understanding of occlusal dynamics and TMJ physiology is paramount for diagnosing, treating, and preventing a spectrum of dental, muscular, and joint disorders. This comprehensive guide will elucidate the fundamentals of occlusion, its critical role in orthodontics, prosthodontics, restorative dentistry, periodontal health, and the cutting-edge principles of neuromuscular occlusion.
Fundamental Concepts: Defining Dental Occlusion
Dental occlusion encompasses the static and dynamic interactions between the maxillary and mandibular teeth, along with their associated neuromuscular and ligamentous components. Beyond simple tooth contacts, occlusion dictates functional harmony between the masticatory muscles, periodontal ligaments, and the TMJ.
- Static Occlusion: The contact between opposing teeth when the jaw is in a stationary, fully closed position.
- Dynamic Occlusion: The manner in which teeth interact during functional movements such as mastication, speech, and deglutition.
A well-balanced occlusion ensures even force distribution, minimizes undue stress on the TMJ, and prevents pathological conditions such as bruxism, malocclusion, and temporomandibular disorders (TMDs). Any deviation from the ideal occlusal scheme can precipitate adverse musculoskeletal and periodontal consequences.
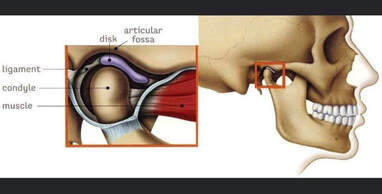
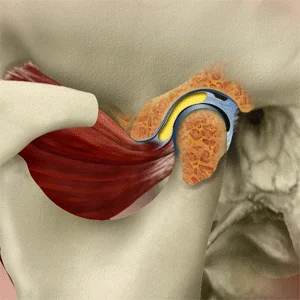
Temporomandibular Joint: A Biomechanical Marvel
The TMJ is a sophisticated, ginglymoarthrodial joint that facilitates both rotational (hinge) and translational (gliding) movements. Essential for critical functions like chewing, speaking, and yawning, the TMJ’s health is intrinsically tied to occlusion.
Key Components of the TMJ:
- Articular Disc: A fibrocartilaginous structure acting as a cushion between the mandibular condyle and temporal bone, ensuring smooth movement.
- Ligaments and Muscles: Provide stability and coordinate movement.
- Synovial Fluid: Lubricates the joint to minimize friction and wear.
The Occlusion-TMJ Relationship: A Bidirectional Influence
Occlusion and TMJ function exhibit a reciprocal relationship:
How Occlusion Affects the TMJ:
- Malocclusion (e.g., deep bite, open bite, crossbite) creates asymmetrical stress on the TMJ, predisposing patients to joint degeneration and dysfunction.
- Premature occlusal interferences induce hyperactivity in masticatory muscles, leading to myofascial pain and disc displacement.
- Overloading specific occlusal contacts can contribute to condylar remodeling and TMJ osteoarthritis.
How TMJ Dysfunction Affects Occlusion:
- Internal derangement of the TMJ (e.g., anterior disc displacement) alters mandibular positioning, resulting in occlusal discrepancies and instability.
- Arthritic changes in the joint can modify condylar height, affecting occlusal vertical dimension (OVD) and interarch relationships.
- TMJ disorders (TMDs) can induce neuromuscular compensations, leading to secondary malocclusion and facial asymmetry.
Key Occlusal Considerations in Clinical Practice
Occlusion Contact Points and Force Distribution
Occlusal contact points dictate load distribution across the dentition. Achieving uniform contact across posterior and anterior teeth ensures optimal force transmission and prevents overloading of specific regions.
- Ideal Static Occlusion: Even, simultaneous contacts in maximal intercuspation (MI) with no premature occlusal interferences.
- Ideal Dynamic Occlusion: Smooth, guided mandibular movements with appropriate disclusion mechanics.
Canine Guidance vs. Group Function
- Canine Guidance: Canines guide lateral excursions, minimizing damaging lateral forces on posterior teeth.
- Group Function: Multiple posterior teeth share occlusal load during lateral movements, beneficial when canines are compromised but increasing posterior tooth wear risk.

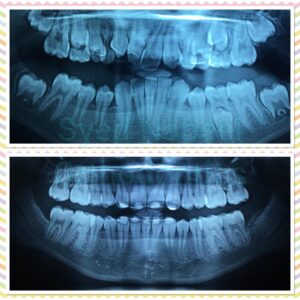
Occlusion in Orthodontics and Malocclusion Correction
Orthodontic treatment aims to achieve a stable occlusion that fosters proper function and aesthetics.
- Class I Occlusion: The ideal molar relationship, where the mesiobuccal cusp of the maxillary first molar aligns with the buccal groove of the mandibular first molar.
- Class II Malocclusion: Anteriorly positioned maxillary molars, associated with retrognathia and increased overjet.
- Class III Malocclusion: Posteriorly positioned maxillary molars, linked to prognathia and underbite.
Malocclusion can exacerbate TMJ dysfunction, contribute to occlusal trauma, and compromise periodontal health.
The Role of Occlusion in Prosthetics and Restorative Dentistry
Achieving proper occlusion is vital in prosthetic and restorative dentistry to ensure long-term stability and function.
- Prosthetics: Dentures, crowns, and bridges must harmonize with occlusal dynamics to prevent instability and excessive wear.
- Restorative Dentistry: Direct and indirect restorations must integrate seamlessly into occlusal schemes to prevent premature contacts, fractures, or dislodgment.
- Implants: Occlusal loading patterns must be carefully controlled, as implants lack the shock-absorbing periodontal ligament.
Occlusion and Periodontal Health: The Role of Biological Width
- Trauma from Occlusion: Excessive occlusal forces can lead to periodontal ligament damage, bone resorption, and tooth mobility.
- Biological Width Preservation: Crown margins should be carefully positioned to avoid impingement on gingival attachment structures.
Centric Relation (CR) and Centric Occlusion (CO): The Cornerstones of Occlusal Stability
- Centric Relation (CR): The condyles’ most superior and anterior position within the glenoid fossa, independent of tooth contact.
- Centric Occlusion (CO): Maximum intercuspation of teeth. Ideally, CO should coincide with CR to prevent occlusal discrepancies.
Neuromuscular Occlusion: A Modern Paradigm
Neuromuscular occlusion considers the entire masticatory system—muscles, nerves, and TMJ—to determine optimal mandibular positioning.
Key Principles:
- Mandibular posture is dictated by muscular balance rather than occlusal contacts alone.
- Establishing a physiologically relaxed musculature reduces TMJ stress and enhances occlusal harmony.
Diagnostic Tools:
- Electromyography (EMG): Evaluates masticatory muscle activity.
- Computerized Mandibular Scanning (CMS): Assesses mandibular trajectory.
- TENS Therapy: Induces muscle relaxation to determine true mandibular rest position.
Conclusion: Mastering Occlusion for Comprehensive Dental Care
The intricate interplay between occlusion and the TMJ underscores the necessity of a holistic, interdisciplinary approach in dentistry. By refining occlusal diagnosis and treatment planning, clinicians can enhance patient outcomes, mitigate TMJ pathology, and ensure long-term oral health.
Key Takeaways:
- Proper occlusion distributes forces evenly, protects the TMJ, and maintains periodontal integrity.
- Malocclusion can lead to TMJ disorders, tooth wear, and functional impairments.
- Occlusion is critical in orthodontics, prosthetics, restorative dentistry, and periodontal health.
- Neuromuscular occlusion offers an innovative approach to achieving functional harmony.
For advanced training in occlusion and TMJ therapy, consider enrolling in specialized courses to elevate your clinical expertise.
WiKiPeDiA PaGe On Occlusion
About the Author
Dr. Syed Nabeel, BDS, D.Orth, MFD RCS (Ireland), MFDS RCPS (Glasgow), is a dedicated dental professional with a special interest in Neuromuscular Dentistry (NMD). With over two decades of experience, he has been committed to diagnosing and managing occlusal and temporomandibular joint (TMJ) disorders using a patient-centered approach that integrates the principles of neuromuscular occlusion.
Alongside his clinical work, Dr. Nabeel is deeply interested in digital dentistry and the role of artificial intelligence (AI) in dental practice. He believes that technology has the potential to enhance patient care by improving diagnostics and treatment precision. His work in this field reflects his curiosity and dedication to advancing dentistry in meaningful ways.
Dr. Nabeel also enjoys sharing knowledge and has been lecturing extensively on neuromuscular dentistry. His approach to teaching emphasizes practical insights, evidence-based methods, and a focus on patient well-being, making his sessions both engaging and valuable for fellow professionals.
Based in Mysore, India, he runs a practice where he strives to combine advanced diagnostic tools with personalized treatment plans to help patients with occlusal and TMJ-related concerns. With a strong commitment to continuous learning and improvement, Dr. Nabeel remains deeply invested in the evolving landscape of dentistry, always seeking ways to enhance patient outcomes with care and compassion.